When arriving at diagnoses and treatment plans, physicians often must look past an individual patient’s particulars to find the commonalities that are at the root of the disease—in other words, to what makes patients the same. Yet this one-size-fits-all approach can lead to suboptimal care, with drugs and other therapies not working as well as expected for many individuals.
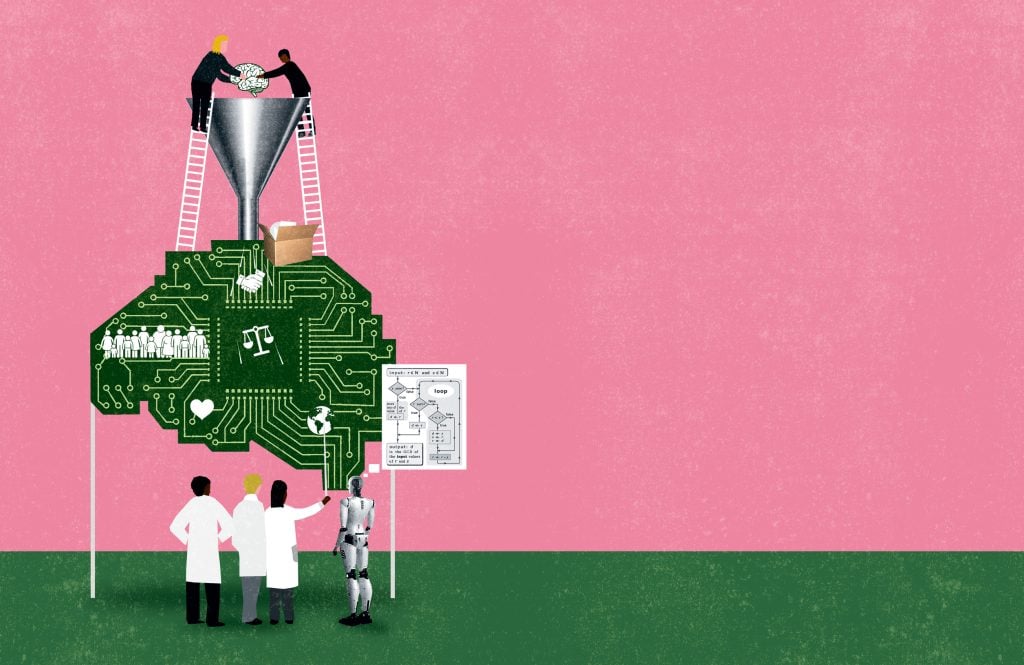
To enhance disease diagnosis and treatment, researchers at the Whiting School of Engineering are instead embracing what makes every patient different. Through advances in data science and AI, reams of patient information can increasingly be gathered by sophisticated yet subtle sensors, both in the clinic and out, and then parsed by algorithms for new insights. In this way, through the development of novel software and hardware, Whiting School researchers are delivering on the promise of precision or personalized medicine—where therapies are tailored to a patient’s unique biology.
Here is one way that data science and AI capabilities are making precision medicine a reality.
MAKING IMAGING EQUITABLE
To improve outcomes for patients with cancer, Muyinatu “Bisi” Bell figured that proactive detection of the disease in its earliest stages, when it is treatable, was the way to go. She accordingly studied medical imaging, assuming it worked identically for all patients. What Bell quickly learned, though, is that some common imaging methods fail to account for normal human variations in skin tone, tissue type, and tissue density.
“I went into imaging thinking this is one solution that benefits everyone equally, but that is not the case,” says Bell, the John C. Malone Associate Professor of Electrical and Computer Engineering.
Take ultrasound and photoacoustic imaging, for example. Both these imaging modalities visualize internal anatomy via the detection of sound waves by sensors in contact with the skin. Ultrasound directly bounces sound off internal tissues, while the photoacoustic method shines laser pulses through the skin, and as bodily tissues absorb this laser energy, they subtly expand and generate ultrasound waves.
“I went into imaging thinking this is one solution that benefits everyone equally, but that is not the case.”
– Muyinatu “Bisi” Bell
For both methods, the timing of the receipt of sound wave signals paints a picture of anatomical locations and physiological features, courtesy of data-processing algorithms. Traditionally, these algorithms are premised on a uniform skin tone and standard ratios of tissue components, such as fat to muscle. Yet the skin of darker-complected individuals absorbs greater amounts of light than that of paler individuals, which scrambles photoacoustic imaging results. Likewise, sound moves differently through the tissue layers of patients with varying fat-to-muscle ratios or different densities of breast tissue. The upshot: Pathological features, such as tumors, can be significantly harder to discern and characterize in Black and brown patients, as well as patients with high or low body mass indexes (BMIs) and tissue densities.
Bell is a pioneer in using data science and AI to remove these biases. She devised a new algorithm rooted in the physics of ultrasound wave propagation that instructs sensors to “talk to their neighbors,” she says. The sensors compare signal receipt timing and cross-correlate data instead of just lumping signals together based on some impersonalized standard. In this way, Bell’s medical imaging algorithm not only constructs a more accurate representation of patients’ internal anatomy, regardless of skin tone, BMI, or tissue density, but also offers greater imaging precision for all patients.
One hitch the new algorithm presents is that its complexity requires additional computing resources. As a solution, Bell has leveraged AI to efficiently speed up processing time by training the algorithm on a wide variety of patient data. “For more individualized imaging that is sharper, clearer, accurate, and faithful to ultrasound physics, these more complex algorithms benefit from AI,” she says.
Overall, the AI-honed algorithm is inexpensive to deploy and still makes imaging results available in real time—both critical elements from a health care delivery perspective, enabling clinicians in rural and remote areas worldwide to immediately inform patients and arrange appropriate follow-up care.
With continuing development, Bell and her colleagues expect to see imaging systems incorporate their approach in coming years. “We’ve shown that it is possible to make imaging technology equitable,” Bell says.
Excerpted from JHU Engineering >>
Illustration by Patric Sandri.