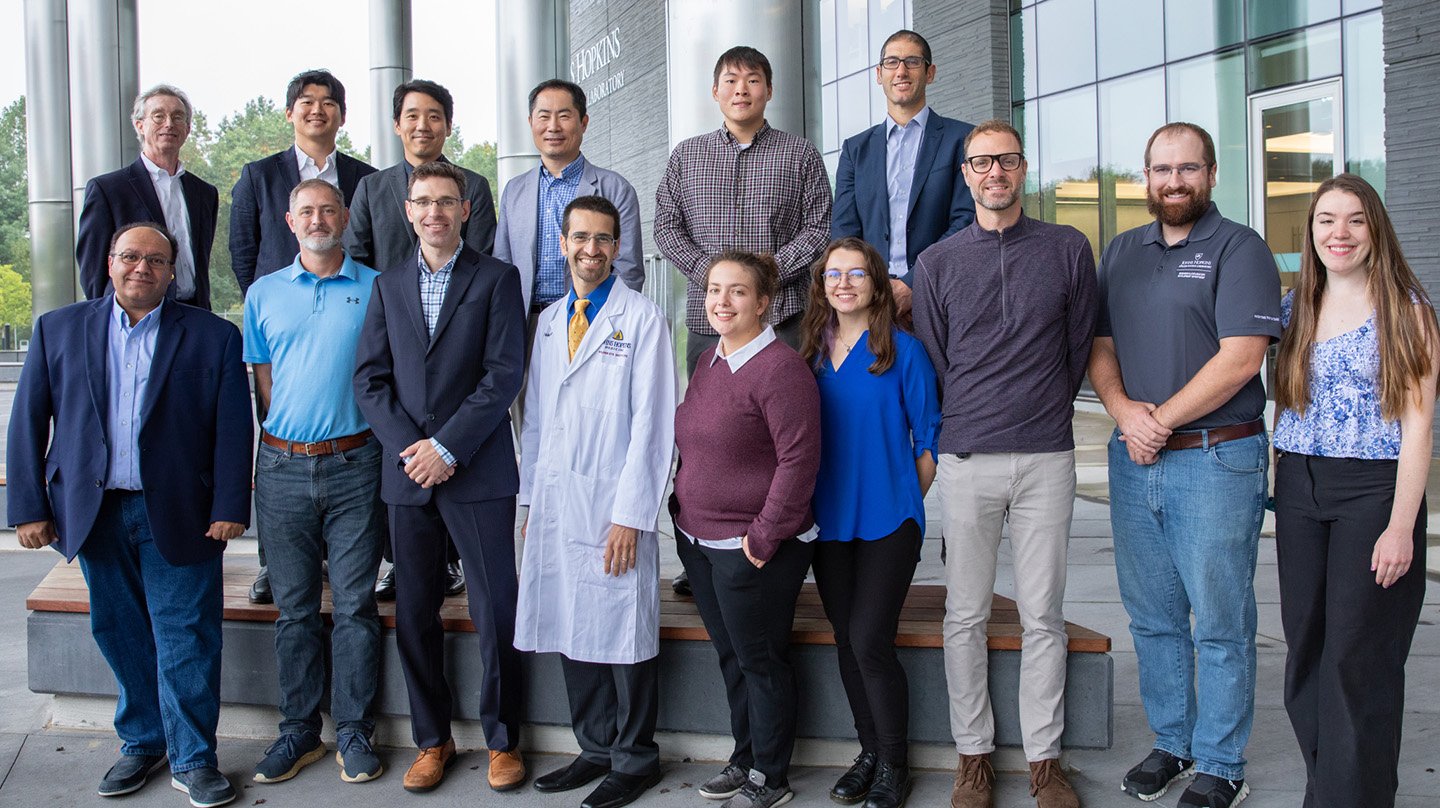
The Photoacoustic Retinal Prosthesis team, from top left: James Spicer (WSE), Hyunwoo Song (WSE), Jeeun Kang (WSE), Jin Kang (WSE), Wayne Rogers (WSE), David Shrekenhamer (APL), Emad Boctor (co-principal investigator, WSE), Luke Currano (APL), Seth Billings (co-principal investigator, APL), Yannis Paulus (SOM), Jacalynn Sharp (APL), Alexandra Patterson (WSE), Chad Weiler (APL), Christopher Stiles (APL), and Erika Rashka (APL). Not pictured: Maomao Chen (SOM), Bree Christie (APL), George Coles (APL), Peter Gehlbach (SOM, WSE), Thomas Johnson (SOM), Dominique Meyer (WSE), Van Phuc Nguyen (SOM), Francesco Tenore (APL), Ji Yi (WSE), Don Zack (SOM), and Mi Zheng (SOM). Image Credit: Johns Hopkins APL / Justin Gladden
Photoacoustic Retinal Prosthesis: A New Paradigm for Prosthetic Vision
Malone affiliate Emad Boctor, the director of the Medical UltraSound Imaging and Intervention Collaboration Laboratory, leads this project with co-PI Seth Billings.
Around 3 million Americans today suffer from irreversible degenerative vision disorders—a figure that is set to double by 2050. The team behind the “Photoacoustic Retinal Prosthesis” project hopes to provide a viable treatment option for individuals suffering from blindness or severe vision loss due to incurable disorders of the outer retina.
To do that, they’re harnessing the power of the photoacoustic effect, a physical phenomenon used in a variety of scientific applications whereby a material absorbs light, heats up, and rapidly expands, generating pressure waves that then propagate as ultrasound. The team’s patented approach—known as photoacoustic retinal stimulation, or PARS—involves using a focused nanosecond pulsed laser to irradiate an implant material to produce ultrasound waves. These waves then stimulate activity within the residual neurons of the inner retina that are responsible for vision. In contrast to existing vision-restoration devices, which require implanting an invasive, active device onto the retina, this approach uses a passive implant that would be stimulated by a wearable device in an eyeglasses form factor.
In its first phase of research under last year’s SURPASS program, the team developed a prototype test device and completed proof-of-concept experiments demonstrating its ability to successfully stimulate activity in retinal neurons.
As the researchers continue their work this year, they’re focused on maturing their technology to improve performance and expand the domain of retinal disorders that could be alleviated with the device, continuing biological studies to further characterize the safety and efficacy of the prototype and optimizing their approach through further experiments.
“No one person or small team can have all of the knowledge and experience that’s required to accomplish something like this,” says co-PI Seth Billings, an APL senior staff scientist. “It takes all of the different divisions of Johns Hopkins coming together.”