Retinitis pigmentosa is a thief, gradually stealing the eyesight of an estimated two million people around the world. Currently, there are no effective treatments to stop or correct the damage caused by this inherited ailment, which kills off photoreceptor cells in the back of the eye.
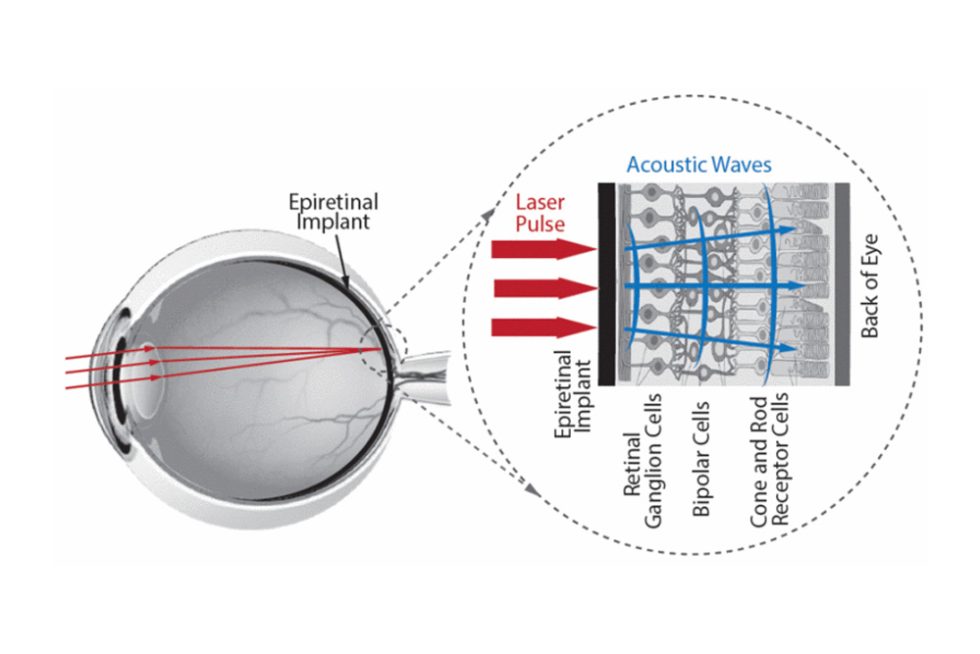
A groundbreaking new material developed by Johns Hopkins researchers could change that. When made into a retinal implant and activated by laser illumination, the biocompatible nanocomposite material shows promise in acoustically stimulating cells in the diseased retina, sending signals to the brain’s visual cortex.
Led by Emad Boctor, an associate research scientist in the Malone Center for Engineering in Healthcare, and Johns Hopkins University Applied Physics Laboratory’s Seth Billings, computer scientist and electrical engineer in the APL’s Research and Exploratory Development Department, a team that also included researchers at the Wilmer Eye Institute and APL presented its results, “Polymer Matrix Nanocomposites as Photoacoustic Transmitters for Epiretinal Prosthetics,” at the 2023 IEEE 23rd International Conference on Nanotechnology in South Korea last summer. Their work is supported by JHU’s SURPASS program, a multimillion-dollar initiative between the Whiting School of Engineering and APL dedicated to using innovative, multidisciplinary approaches to solve some of the world’s most pressing problems.
“Though there is a long way to go, the immediate application for our materials is to produce a retinal prosthetic that can be used to produce what we call a ‘vision-like’ experience for patients suffering from a loss of vision,” said research team member Alexandra Patterson, a graduate student in the Whiting School’s Department of Materials Science and Engineering, who worked on the project with Materials Science and Engineering Professor James Spicer. “But there are also potential applications for this material in other areas of medicine, as well as in energy production, precision measurements, and imaging.”
The soft, flexible material developed by the team contains nanoparticles of a metal called palladium, which can convert light into sound waves that activate retinal cells. Using a special technique that let them grow the particles directly inside a silicone matrix ensured that the resultant material would be capable of producing strong, stimulating sound waves when exposed to low-power pulses of light.
The team used X-ray diffraction and transmission electron microscopy to confirm the size and arrangement of palladium particles within the silicone matrix and then assessed its optical properties using a spectrophotometer, a tool that measures how a sample absorbs or transmits light.
“We learned that for this application, the materials must be biocompatible, stable, and robust when exposed to the laser—a set of characteristics that is challenging to achieve,” said Patterson. “Enhanced performance in one area can mean degraded performance in another.”
Currently, other members of the team are testing how the material interacts with retinal cells, while Patterson and Spicer are exploring transforming their novel material into a specific curved shape.
“All of our materials so far have been flat, so our next efforts will be to develop one that will follow the contours of the human retina while maintaining the desirable characteristics of the implant material,” she said.
Billings, whose team at APL spans focus areas across AI, computer vision, and optical systems, with applications in autonomy, robotics, rehabilitative technology, and interventional and diagnostic medicine, said the advances being made by this research group “are a key pillar in our strategy for leveraging photoacoustics to treat incurable blindness caused by degenerative retinal disorders. This material will not only enhance the stimulation effect that we can achieve using photoacoustics but will also play the dual function of shielding the sensitive tissues of the retina from direct laser exposure.”
Image Caption: Schematic of photoacoustic retinal stimulation using an epiretinal implant that serves as a photoacoustic transmitter when excited by the output of a pulsed laser system. The implant prevents light penetration to the retina and converts the laser pulse into an acoustic pulse that excites retinal cells.